-
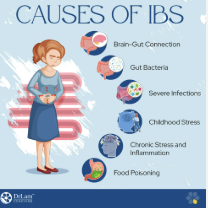
Gut Microbiome Imbalance (Dysbiosis)
A disrupted balance between beneficial and harmful gut bacteria can lead to bloating, gas, inflammation, and digestive discomfort. Contributing factors include antibiotic use, chronic stress, and poor dietary habits.
-
Food Sensitivities and Intolerances
Many individuals with IBS react to specific foods such as gluten, dairy, or high-FODMAP foods. Targeted testing can help identify triggers and significantly reduce symptoms.
-
Chronic Stress and Nervous System Imbalance
The gut-brain axis links emotional wellbeing and digestive function. Ongoing stress, anxiety, or trauma can disrupt gut motility, increase sensitivity, and worsen IBS symptoms.
-
Hormonal Fluctuations
Hormonal changes, particularly in women, can influence gut motility and microbiome balance. Fluctuations in estrogen and progesterone may trigger or exacerbate IBS symptoms.
-
Poor Diet and Nutrient Deficiencies
Diets high in processed foods, low in fibre, or lacking essential minerals can impair digestion and detoxification. Supporting nutrient balance is key to restoring healthy gut function.
-
Post-Infectious or Inflammatory Triggers
IBS can develop after gastrointestinal infections, antibiotic use, or inflammatory conditions that compromise gut integrity, leading to ongoing digestive sensitivity.
Frequently Asked Question
Q: If my condition improves, will it stay that way? I don’t want to go through this again.
A: This is a very valid concern Pratica e fresca t-shirt. Many people who recover from IBS or SIBO may remain symptom-free if they continue to follow the strategies implemented during treatment. However, IBS often comes with a predisposition to gut sensitivity. If you return to previous lifestyle habits or stress patterns, relapses can occur. Long-term success depends on maintaining dietary, lifestyle, and stress-management practices for gut health.